For decades, biological psychiatric research, in particular psychiatric
genetics, has been based on cross-sectional data sets without paying much attention to a
phenotype that is of utmost relevance to both the clinician and the patients and their
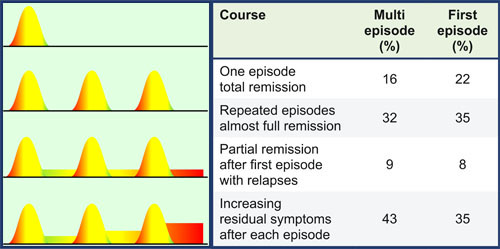
family members: the longitudinal course. From several epidemiological studies we know
that there are characteristic types of the longitudinal course of schizophrenia. These
types are defined both by the pattern of relapse and by levels of impairment. Impairment
due to negative symptoms such as blunted affect, avolition, alogia, or anhedonia has been
found associated with a reduced ability to earn one's living, which can be taken as a
surrogate marker for social functioning of an adult in our western societies. Overall 20 %
of the patients presenting an episode of schizophrenia will totally remit. Around 30 % will
have several episodes, but completely remit between each episode. 10 % of the patients will
have a remitting course with a stable deficit. The remaining 35 to 45 % of the patients
mirror the core problems of this disorder. Patients will have a remitting course but, from
relapse to relapse, their residual symptoms will increase and hinder the sufferers to cope
with their disabilities. The effect consists in frequent relapses precluding the patients
from fulfilling their psychosocial goals. Only 20 % of all patients with schizophrenia have
regular work and only 30 % are able to keep up a stable relation. In a current large-scale
study on first-episode schizophrenia, the effect of different neuroleptics on psychopathology,
cognition, and adherence to medication was examined. Most of the patients remained on the
atypical neuroleptic amisulpride, while least on the typical substance haloperidol. There
is a subgroup of patients (20 %) recovering from schizophrenia, irrespective of the
administration of an antipsychotic. For another 30%, neuroleptic treatment, irrespective
of the choice of substance, is important for fair recovery. We are left with around 50 %
of the patients, for whom neuroleptics seem to ameliorate symptoms but do not lead to a
substantial remission of complaints. Beside neuroleptics, any other intensive care system
for first break schizophrenia, as demonstrated by the
OPUS-trial,
did not overcome this longitudinal outcome pattern.